Home > Pharmacy > Medicare Advantage > 2026 MA Pharmacy Gundersen MN
2026 Pharmacy Coverage
Gundersen Minnesota Quartz Medicare Advantage
Understanding what Quartz covers and what you'll pay for drugs
Quartz Medicare Advantage (HMO) offers several plan options with prescription drug benefits (Rx) coverage. These plans cover Part D drugs and Part B drugs.
2026 prescription drug coverage
Quartz Medicare Advantage has a list of all covered drugs (formulary) that you can view in a printable document. Refer to our top-drug categories list to see the most common preferred and non-preferred drugs.
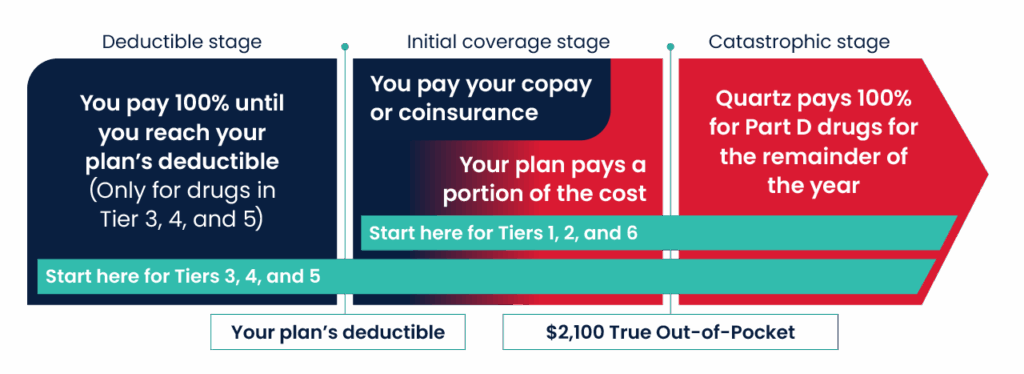
- There is a deductible for Tiers 3, 4, and 5 prescription drugs. Basic D: $270; Core D: $270; Value D: $225; Elite D: $200.
- These costs apply until the member’s True Out-of-Pocket (TrOOP) amount reaches $2,100, the maximum they will pay out-of-pocket.
- Covered drugs can be filled at network retail or mail-order pharmacies.
|
|
Deductible applies?
|
Your share
|
30-day
|
31 to 60-day
|
61 to 100-day
|
|---|---|---|---|---|---|
|
Tier 1 (Preferred Generic) |
× No |
Copay |
$2 |
$4 |
$5 |
|
Tier 2 (Generic) |
× No |
Copay |
$10 |
$20 |
$25 |
|
Tier 3* (Preferred brand) |
✓ Yes |
Coinsurance |
20% |
20% |
20% |
|
Tier 4 (Non-preferred drugs) |
✓ Yes |
Coinsurance |
40% |
40% |
40% |
|
Tier 5** (Specialty) |
✓ Yes |
Coinsurance |
30% retail only |
Not available** |
Not available** |
|
Tier 6*** (Select Care drugs) |
× No |
Copay |
$0 |
$0 |
$0 |
*Tier 3 includes many common brand-name drugs, some higher-cost generic drugs, and insulin.
**Tier 5 (Specialty) 30-day supply available in retail locations only. Not available through mail-order pharmacy benefit.
***Tier 6 includes many low-cost medications that treat diabetes, high blood pressure, high cholesterol, osteoporosis, and other conditions.
This plan is available in these Minnesota counties: Filmore, Houston, Olmstead, and Wabasha.
Note: Our plan covers Part D vaccines (e.g., Tetanus (Tdap), shingles, etc.) at no extra cost, even if your plan has a deductible and you haven’t paid it. There is no extra cost for vaccines received in a pharmacy. You will need to submit a reimbursement form for vaccines received in a clinic.
Diabetic testing supplies
Preferred blood glucose meters and test strips
The Accu-Chek product line is the preferred manufacturer of blood glucose meters and test strips, and these are covered at $0 cost-sharing. Other brands of test strips are not covered unless we approve an exception. Test strips are limited to 200 strips per 30 days.
Preferred continuous glucose monitors (CGMs)
FreeStyle Libre 2, FreeStyle Libre 3, Dexcom G6, and Dexcom G7 are the preferred continuous glucose monitors when submitted through the pharmacy benefit manager (PBM) and are covered at a 10% cost-sharing. Prior authorization is not required if the member has had a paid claim for insulin through the PBM in the past six months. Members that have not had a paid claim for insulin through the PBM in the past six months will require prior authorization for coverage.
Check drug price
To check drug prices, log in to QuartzMyChart.com and click Pharmacy Benefits.
Don’t have a Quartz MyChart account? Use the QuartzRx drug price search (Note: if using this link, the pricing won’t include any applicable deductible, and it will return initial coverage phase pricing.)
Helpful resources for your pharmacy and prescription needs
Exceptions to the formulary
The formulary is the list of medications covered by Quartz Medicare Advantage (HMO). If a member needs a medication that isn’t on the formulary, first consider whether another covered drug might work just as well — your provider can help review options.
If no suitable alternative is available, a formulary exception request may be an option.
When an exception may be needed
An exception can be requested when:
- Non-formulary drug: The medication isn’t covered by the plan, and no suitable alternative is available.
- All similar formulary drugs would not be effective
- Formulary drugs would cause harmful side effects
- Coverage restrictions: The drug is covered but has limits, such as:
- Step therapy – You may need to try a different drug first to see if it works before the requested drug can be covered.
- Quantity limit – There may be a maximum number of tablets or doses covered per day.
- Tier exception: The drug is covered, but it is in a non-preferred cost-sharing tier.
If you’re a current member and a medication you take will be removed from the formulary or restricted in some way for the upcoming plan year, you can request an exception in advance. In these instances, the request must specify that it is a “Predetermination Request.” We will review your request and provide an answer before the change takes effect.
Common tier exception requests
- Tier 4 (Non-preferred drugs) – A provider can ask us to cover the medication at the lower cost-share that applies to formulary alternatives in a lower cost-sharing tier, if applicable.
- Tier 2 (Generic) – A provider can ask us to cover the medication at the lower cost-share that applies to formulary alternatives in Tier 1, if applicable.
Tier exceptions are not allowed for
- Specialty drugs (Tier 5) are not eligible for tier exceptions.
- Brand drugs to be covered at a lower tier when there is not a brand drug alternative covered at that tier.
- Brand or generic drugs when there are no formulary alternatives covered at a lower tier.
- Biological products to be covered at a lower tier when there is not a biological alternative in that tier.
Requesting an exception
If there is a medical reason why a member needs a drug outside the formulary or its restrictions, a provider can submit a Coverage Determination Request to ask for an exception. Quartz Medicare Advantage will review the request and determine whether coverage can be approved.
If we approve your request for a non-formulary medication, it will be covered at a Tier 4 (Non-preferred drug) copay.
Low-Income Subsidy
Medicare offers programs to help members with limited income and resources pay for prescription medications. If you qualify, you may receive Extra Help through the Medicare Part D Low-Income Subsidy (LIS) program.
How to apply for Extra Help
You can learn more or apply for the Medicare Part D Extra Help program through:
- The Social Security Extra Help page (By clicking this link, you will leave the Quartz Medicare Advantage website.)
- Social Security at (800) 772-1213 (TTY: (800) 325-0778)
Quartz Part D Low-Income Subsidy premiums
If you qualify for the Part D Low-Income Subsidy, your monthly premium may be reduced depending on your plan and the level of Extra Help you receive.
2025 premiums if your level of Extra Help is 100%
- Core D: $0.00
- Value D: $31.70
- Elite D: $80.50.
2026 premiums if your level of Extra Help is 100%
- Basic D: $0.00
- Core D: $4.60
- Value D: $67.70
- Elite D: $174.60.
Verifying eligibility with Best Available Evidence (BAE)
If you qualify for Extra Help but are paying a higher copayment, Quartz Medicare Advantage can help confirm your eligibility through Medicare’s Best Available Evidence (BAE) Policy. (By clicking this link, you will leave the Quartz Medicare Advantage website.)
You can verify eligibility by providing one of the following documents:
- Copy of your Medicaid card (showing your name and eligibility date)
- State document confirming active Medicaid status
- Printout from the state’s electronic enrollment file showing Medicaid status
- Screen print from the state’s Medicaid system confirming eligibility
- Other state documentation provided by the state showing Medicaid status
- Social Security Administration (SSA) letter showing you receive Supplemental Security Income (SSI)
- Important Information letter from SSA confirming automatic Extra Help eligibility
If you have these documents, contact your Quartz Champion for assistance.
Institutionalized members
Members who live in a care facility may qualify for $0 cost-sharing. To verify eligibility, Quartz Medicare Advantage must provide Medicare with one of the following:
- Facility remittance showing Medicaid payment for a full calendar month
- State document confirming Medicaid payment to the facility for a full month
- Screen print from the state’s Medicaid system showing institutional status for a full calendar month
Transition fills
If a member takes a drug that is not on the formulary (drug list) or is listed as restricted in some way (for example, requires prior authorization), they may qualify for a temporary supply called a transition fill.
A transition fill allows members to continue their medication without interruption while they and their doctor decide on the next steps. Options may include switching to a covered alternative or submitting a Coverage Determination Request to Quartz Medicare Advantage to request continued coverage.
How transition fills work
When a member receives a transition fill, Quartz sends a letter to both the member and their prescriber explaining that the supply is temporary.
To qualify, both of the following must apply:
- The drug coverage change must be one of the following:
- Drug is no longer on the plan’s formulary (drug list)
- Drug is now restricted in some way
- One of the following member situations applies:
- New members (not in a long-term care facility): Eligible for a one-time, up to 30-day supply (or less if prescribed for fewer days) during the first 108 days of coverage.
- New members in a long-term care facility: Eligible for an initial up to 31-day supply (or less if prescribed for fewer days), with additional refills available as needed during the first 108 days of coverage.
- Current members (in a long-term care facility): If immediate access to a non-formulary or restricted drug is needed, one 31-day supply (or less if prescribed for fewer days) will be covered in addition to the transition supply described above.
Questions?
For more details, review the Quartz Medicare Advantage Part D Drug Transition Policy or contact your Quartz Champion.
You may also call using a video relay service of your choice. Interpreter services are provided free of charge to you.
We’re here for you.
Thanks for choosing Quartz Medicare Advantage. If you have questions or need support, your local Quartz Champion is here for you.
